ET Tube Stabilizer : Research for a next generation Endotracheal Tube Holder
This project focused on researching and refining the first prototype of an endotracheal (ET) tube holder , a device designed to stabilize airway tubes during intubation. Since the product had not yet undergone clinical testing, our goal was to evaluate its usability, fit, and maintenance feasibility before further development.
Project Summary
Context
10XBETA
Timeline
4 Weeks
Collaborators
Product Manager, Industrial Designer, Firmware Engineer
UX Research / Human Factors
Responsibilities
This project focused on researching and validating potential improvements to an endotracheal (ET) tube holder — a critical device used to secure airway tubes for patients who cannot breathe on their own. When I joined, the first prototype of a strap-based, adhesive-free ET tube holder had been developed but not yet tested in clinical settings. The team wanted to explore two key questions before the next design iteration:
1. Adapt to different patient anatomies, ensuring proper fit across faces of various sizes and structures.
2. Withstand real hospital cleaning and maintenance workflows, ensuring hygiene, reusability, and long-term safety.
3. Should a bite block be integrated into the holder to simplify workflows and reduce the number of devices used during intubation?
The prototype’s core innovation was :
1. Bidirectional swivel mechanism — allowing tube rotation to both sides for flexible patient repositioning.
2. Extended-length holder body — improving tube grip and reducing accidental extubation risk.
3. Potential bite block integration — to reduce oral device clutter and simplify workflow.
In parallel, I led research to map the complete clinical workflow — from intubation to cleaning and re-use — to uncover pain points and guide usability, hygiene, and fit decisions.
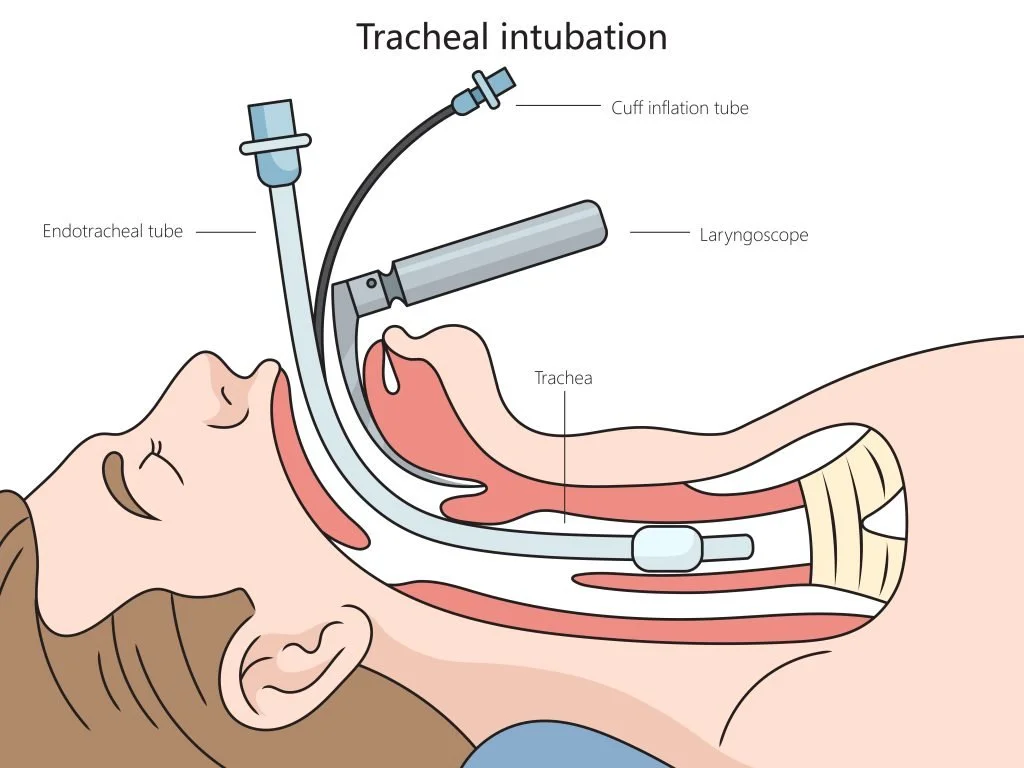
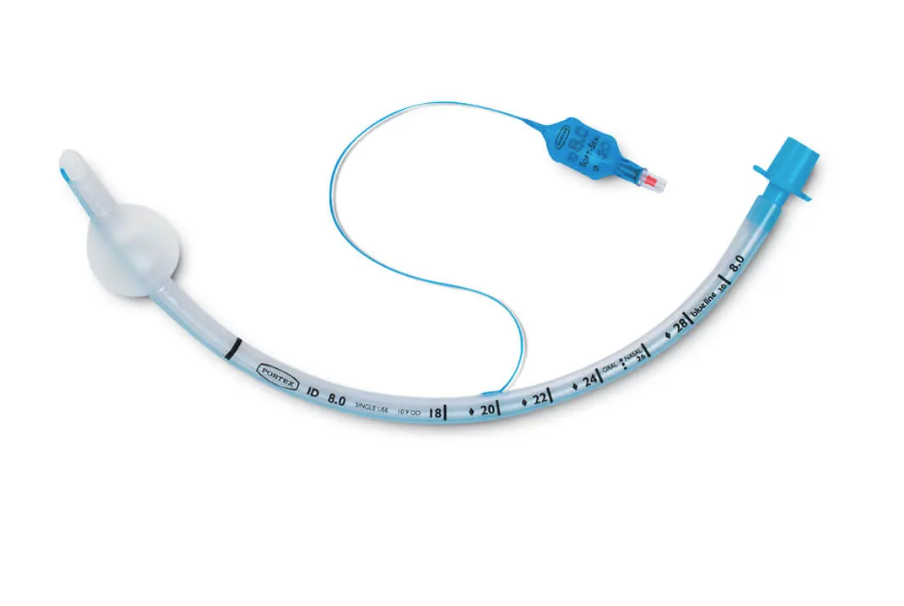
Endotracheal (ET) tubes are used to intubate patients who cannot breathe on their own, such as those under anesthesia or on ventilator support in intensive care. The tube is inserted into the trachea to maintain an open airway, a procedure that is life-sustaining but fragile.
Because the human body has a natural gag reflex, and sedated or unconscious patients can still move involuntarily, the ET tube is at constant risk of accidental extubating (unplanned removal). To prevent this, hospitals use tube holders or stabilization systems that secure the tube in place while minimizing discomfort and pressure on the patient’s face.
Overview
Why is an ET Tube Stabilization System Important ?
Once an ET tube is inserted, it must remain precisely positioned inside the trachea.
If the tube slips out a situation known as accidental extubation, the patient can lose their airway within seconds, leading to oxygen deprivation, lung injury, or even death.
Because the human body has natural gag and cough reflexes, and patients often move involuntarily even under sedation, the ET tube needs to be securely stabilized outside the mouth.
That’s where the ET stabilization system (or tube holder) plays a critical role.
Prevents accidental extubation - keeps the airway sealed and secure during patient movement.
Reduces reliance on tape or improvised methods, which can loosen with moisture or cause skin irritation.
Improves workflow efficiency - allows nurses and respiratory therapists to quickly adjust or check tube position.
Enhances patient comfort and safety - distributes pressure evenly to minimize facial injury or sores during long ventilation periods.
Supports infection control - reusable systems designed for proper cleaning lower contamination risk.
In short, a well-designed ET stabilization system ensures that a patient’s ability to breathe — and survive — is not compromised by device failure or poor usability.
Accidental extubation is one of the most common and preventable ICU emergencies. A reliable stabilization system keeps the airway and the patient safe.
Problem Statement
While the initial prototype eliminated adhesive-related irritation, it was still unclear if it fully addressed ergonomics, cleaning efficiency, and workflow flexibility.
Existing market holders were adhesive-based and could only swivel in one direction, limiting how clinicians repositioned patients or managed ventilator tubing. Our research focused on validating whether a non-adhesive, bidirectional, longer strap-based holder could improve safety, comfort, and hygiene without introducing new complexities.
Research Goals
Assess usability, fit, and comfort across patient profiles.
Understand cleaning and maintenance workflows in ICU and OR environments.
Evaluate user needs for rotation, reusability, and ergonomics.
Gather clinical feedback from nurses, respiratory therapists (RTs), and physiotherapists (PTs).
Translate findings into actionable design directions for iteration 2.
Secondary Research
1. Competitive Analysis
I reviewed the leading ET tube holders (Anchorfast, Dale, Thomas Tube) and studied FDA and CDC guidelines for reprocessing semi-critical devices. I also examined anthropometric datasets to understand variation in adult facial dimensions.
Key Findings
Most holders rely on adhesive cheek pads (Anchorfast), which irritate skin and are single-use.
One-way swivels hinder suctioning and patient repositioning.
Tape is also another medium used to secure the tube in place.
🧠 Insight: A universally adaptable, strap-based holder with bidirectional movement and durable, cleanable materials could significantly improve clinical performance.
2. Survey Study
I surveyed 12 clinical providers, a mix of Respiratory Therapists and Paramedics.
Insights :
All of the clinicians used some form of a ET Tube holder as a securement device. Mostly anchorfast.
70% found their current device to be functioning well or satisfactorily.
40% found it challenging to fasten and unfasten the holder.
Clinicians also found that the current holder that use to be moderately secure.
Another insight was the inconsistency in inline suctioning - while some providers performed inline suctioning every 2-4 hours , most of the providers performed it when necessary.
(Inline Suctioning - is a medical procedure to clear secretions from the airway of a patient with a tracheostomy or endotracheal tube.)
3.Workflow Analysis
(insert visual: Service Blueprint of Cleaning and Maintenance after an Intubation)
After researching thoroughly through primary and secondary methods, I mapped the end-to-end journey of an ET tube and holder through hospital workflows to identify friction points.
Frontstage: Intubation, tube securing, patient repositioning.
Backstage: Cleaning, drying, reuse labeling.
Findings:
Adhesive components from other systems made reuse nearly impossible.
Access to the all part of the tube was crucial to prevent the patient from developing Pneumonia since they are vulnerable during this time.
Outcome: Workflow mapping showed that cleaning inefficiencies and unclear reprocessing ownership were major barriers to device consistency and safety.
4. Field Interviews
I conducted semi-structured interviews with:
2 ICU Nurses
2 Respiratory Therapists
We explored how a patient is intubated, Challenges during Intubation and Post Intubation, Cleaning and Maintenance routines.
Insights from Interviews :
Adhesive holders peel off when the patient sweats , especially long-term cases. The adhesive also leaves pressure ulcers on the patients face.
Cleaning and Maintenance schedules vary from hospital to hospital as well as the use of holders. Some hospitals do not use any holders, rather just use tape to secure the tube.
Cleaning agents also varied as per hospital policies, no standardization in terms of workflow.
Not all hospitals use bite blocks for their patients, plus bite blocks are breeding grounds for bacterial and potential infections.
Insight : The lack of flexibility and adhesive-related discomfort were consistent pain points.Anthropometric Evaluation
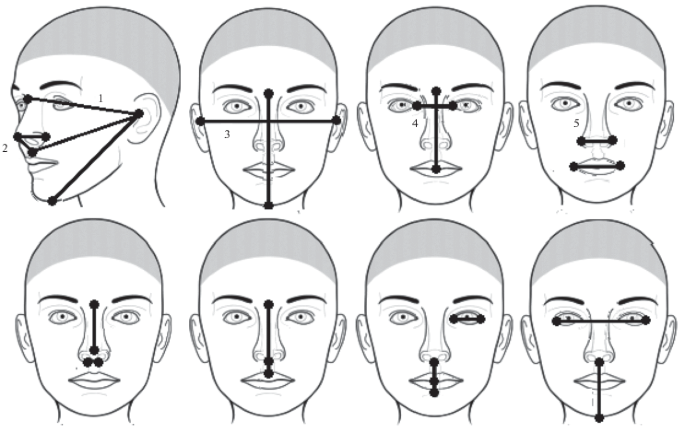
5. Anthropometric Research
I researched for facial dimension data (NIH datasets) to assess fit ranges.
Findings:
Most existing holders fit ~70% of adult faces.
The new strap-based concept covered a broader range but required softer contact zones to prevent cheek pressure.
The extended-length holder design improved grip and minimized dislodgement potential during patient movement.
Insight: The longer design and modular straps improved both security and comfort — reducing the likelihood of accidental extubation.
From Research to Design Direction
My research validated the next prototype’s core design strategy:
Adhesive-Free Comfort: Strap-based stabilization using soft, skin-safe materials.
Bidirectional Swivel: Full tube rotation on both sides for clinical flexibility.
Extended-Length Holder: Longer clamp body for enhanced stability and reduced extubation risk.
Bite Blocks : Design an optional, detachable bite block for modular integration.
Materials : Refine materials for smooth surfaces and chemical resistance to withstand enzymatic cleaners.
Impact
Even before clinical validation, this research established the foundation for engineering and testing the next-generation holder:
Validated longer design geometry for better extubation prevention.
Confirmed user preference for non-adhesive materials.
Created alignment between design, engineering, and clinical teams.